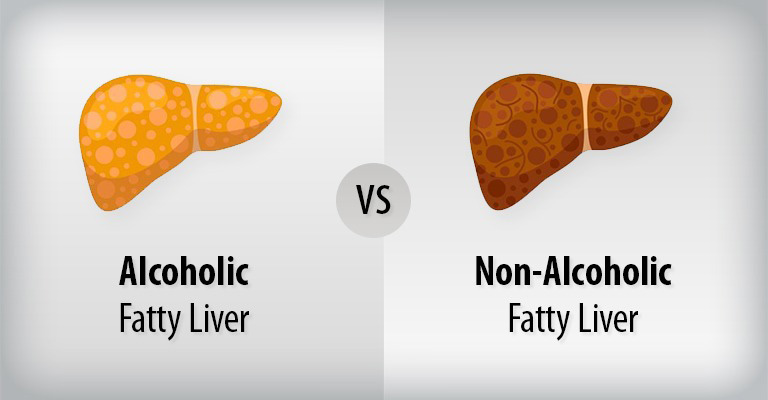
Nonalcoholic steatohepatitis (NASH) is a liver ailment marked by inflammation and harm caused by the buildup of fat within the liver. As part of the nonalcoholic fatty liver disease spectrum, NASH can result in complications when not addressed.
In this blog, we’ll delve into the causes, symptoms, diagnosis, and treatment of NASH.
What is Nonalcoholic Steatohepatitis (NASH)?
NASH develops when excess fat in the liver triggers inflammation and damages liver cells. Though many people may have a fatty liver without experiencing symptoms, some individuals may suffer from liver dysfunction due to this fat buildup.
Unlike liver diseases associated with alcohol abuse, NASH occurs in individuals who do not misuse alcohol.
Symptoms of Nonalcoholic Steatohepatitis (NASH)
During the early stages, NASH may not present noticeable symptoms. However, as liver damage progresses, symptoms may include fatigue, unexplained weight loss, general weakness, and discomfort in the upper right part of the abdomen.
It can take several years for NASH to advance to a stage where symptoms become apparent.
Causes of Nonalcoholic Steatohepatitis (NASH)
The exact cause of NASH remains unclear, but factors such as environmental triggers or genetic predisposition may contribute.
Risk factors for NASH and associated liver damage include obesity, insulin resistance, type 2 diabetes, high cholesterol, high triglycerides, and metabolic syndrome.
While most individuals with NASH are between 40 to 50 years old and have these risk factors, the condition can also occur in those with none of these risk factors.
Diagnosing Nonalcoholic Steatohepatitis (NASH)
There is no single test for diagnosing NASH. Healthcare professionals rely on a combination of tests, including blood tests, abdominal ultrasound, CT scan, and MRI scan, to assess fat buildup in the liver and rule out other diseases. In some cases, a liver biopsy may be conducted to confirm the presence of NASH by examining liver tissue.
Treatment for Nonalcoholic Steatohepatitis (NASH)
Managing conditions that contribute to or worsen NASH is key to treatment. This includes reducing total cholesterol levels, achieving a healthy weight (with a 3% to 10% body weight loss making a significant impact), controlling diabetes, and limiting alcohol intake. Regular exercise is also recommended to support overall liver health.
Conclusion
Nonalcoholic Steatohepatitis (NASH) is a complex liver condition that requires careful management and attention to associated risk factors.
Understanding the causes, recognizing symptoms, and undergoing proper diagnosis are crucial steps in addressing NASH and working towards a healthier liver.
If you suspect you may have NASH or are at risk, consult with our Best Hepatologist at Medica North Bengal Clinic for personalized guidance and care.